ACEs Aware Progress Report: 2019-2023
To read an executive summary of the report, scroll through this page.
Access the full report:

One of my proudest accomplishments as California Surgeon General was to launch the ACEs Aware initiative, in partnership with the Department of Health Care Services (DHCS)…We set out to raise awareness in the health care community and build capacity for providers to prevent, identify, and respond to ACEs and toxic stress with evidence-based, cross-sector and coordinated interventions… While there continues to be much work ahead, I have the utmost confidence that, together, we can interrupt the progression from early adversity to disease and early death.
Adverse Childhood Experiences (ACEs) impact everyone, cutting across different backgrounds like ethnicity, socioeconomic status, gender, and location. In California, over 70 percent of adults and 30 percent of children have faced at least one ACE, such as having a caregiver with mental health challenges or witnessing domestic violence. Shockingly, 1 in 5 adults has encountered four or more ACEs. The science now reveals that the toxic stress response is a key biological factor causing ACEs to lead to long-term health issues affecting individuals and communities statewide… The good news is that ACEs are not predetermined. Research indicates that early detection and evidence-based interventions can significantly reduce negative outcomes.
Fast Facts
Impacts of Adverse Childhood Experiences and Toxic Stress
Prevalence of ACEs in California — Adults1
Prevalence of ACEs in California — Youth (Ages 0–17)2
Estimated Annual Cost of ACEs to State of California3
Annual Cost of ACEs in the U.S.4
Population-Attributable Fractions of ACEs for Health Outcomes in North America5
ACEs Dramatically Increase Risk for at least 9 of the 10 Leading Causes of Death in U.S.6
Odds Ratios for ≥ 4 ACEs (Relative to no ACEs)
ACEs Aware Progress on Addressing ACEs and Toxic Stress
ACE Screening by Medi-Cal Providers
Becoming ACEs Aware in California Training
Investing in California Communities
ACE Screening Impact on Access to Services7
ACE Screening is improving Medi-Cal members' access to services
Primary care quality outcomes in clinics within the LA Department of Health Services (LA DHS) that screen for ACEs suggest that access to health care services is expanding for patients who are screened for ACEs (compared to clinics that do not screen).
Health Care Access
Primary Care Quality
Improvement in Clinical Outcomes
Increased Identification for Pediatric Enhanced Care Management (ECM)
Improving Health Care Access and Quality in LA County: The ACEs-LA Network of Care Case Study Early findings in Los Angeles County suggest that ACE screening and response initiatives are advancing DHCS’ statewide goals to improve quality of care and reduce health disparities for the most vulnerable Californians. Read the case study →
Early findings in Los Angeles County suggest that ACE screening and response initiatives are advancing DHCS’ statewide goals to improve quality of care and reduce health disparities for the most vulnerable Californians. Read the case study →
ACEs and Toxic Stress
ACEs are adversities experienced prior to age 18 that were categorized in the landmark 1998 study by the Centers for Disease Control and Prevention (CDC) and Kaiser Permanente.8 They include 10 categories of adversities in three domains: child abuse (physical, emotional or sexual), neglect (physical or emotional), and/or household challenges (growing up in a household with incarceration, mental illness, substance misuse or dependence, parental separation or divorce, or intimate partner violence).
Abuse
Neglect
Household Challenges

A consensus of scientific evidence points to cumulative adversity, especially when experienced during critical and sensitive periods of development, as a root cause of some of the most harmful, persistent, and expensive health challenges facing our state and nation, from heart disease to homelessness. Research confirms that exposure to ACEs, along with other adversities, may lead to prolonged activation of the biologic stress response, which can lead to long-term disruption of neurologic, immune, metabolic, and endocrine systems, as well as changes to genetic regulatory mechanisms. Together these changes constitute the toxic stress response.
Through the toxic stress response, ACEs significantly increase risk for harmful health conditions, including 9 of the 10 leading causes of death in the United States.9 ACEs are common, with 72 percent of California adults experiencing at least one ACE and 20 percent experiencing 4 or more. ACEs are expensive, costing the state of California an estimated $1.5 trillion annually — $24.6 billion in direct medical spending, and $1.49 trillion in lost healthy life years.10 ACEs, which are disproportionately concentrated in racially, socially, and economically marginalized communities, contribute to health disparities.
The good news is toxic stress is a health condition amenable to treatment. Scientific data suggest that early detection and intervention improve health outcomes.
ACEs Aware Background
As one of his first acts in office, Governor Gavin Newsom established the Office of the California Surgeon General (CA-OSG) and appointed Dr. Nadine Burke Harris as California’s first Surgeon General. She was charged with addressing the root causes of persistent health inequities among Californians and set as her top priorities ACEs and toxic stress, early childhood, and health equity. As the foundation for this work, the newly established CA-OSG and the DHCS launched ACEs Aware in 2019, a first-in-the-nation initiative to promote early detection and intervention for ACEs and toxic stress.
ACEs Aware was launched with the goal of significantly reducing ACEs and toxic stress in children, adults, and families by training health care teams to screen and respond to ACEs and toxic stress and catalyzing the development of Trauma-Informed Networks of Care to support stronger ties between health care settings and community partners. ACEs Aware is bringing communities together in ways never before imagined to prevent, screen for, and treat toxic stress, reducing the risk of intergenerational transmission of ACEs and of toxic stress and averting their significant health and societal consequences.
Addressing ACEs and toxic stress through the ACEs Aware initiative is a key health equity activity in DHCS’ Comprehensive Quality Strategy (CQS), part of a 10-year vision for Medi-Cal transformation to ensure high-quality and equitable care for all Medi-Cal members. As outlined in the Roadmap, “social and structural inequities disproportionately concentrate ACEs, toxic stress, their precursors, and their consequences in racially, socially, and economically marginalized communities. Such contexts can exacerbate the impact of ACEs and toxic stress.”

DHCS Quality Strategy Goals
Quality Strategy Guiding Principles
- Eliminating health disparities through anti-racism and community-based partnerships
- Data-driven improvements that address the whole person
- Transparency, accountability, and member involvement
With oversight from DHCS and CA-OSG, the UCLA-UCSF ACEs Aware Family Resilience Network (UCAAN) is charged with implementing the ACEs Aware initiative. UCAAN is a multi-campus health equity initiative that leverages the substantial interdisciplinary resources of the University of California, Los Angeles (UCLA) and the University of California, San Francisco (UCSF) to advance the mission of ACEs Aware by building on the evidence base to develop statewide, sustainable capacity for ACE screening and response. This innovative partnership brings together scientific rigor, education and training resources, and clinical expertise, ensuring that scientific evidence is the foundation for ACEs Aware.
Progress and Impact
ACE Screening
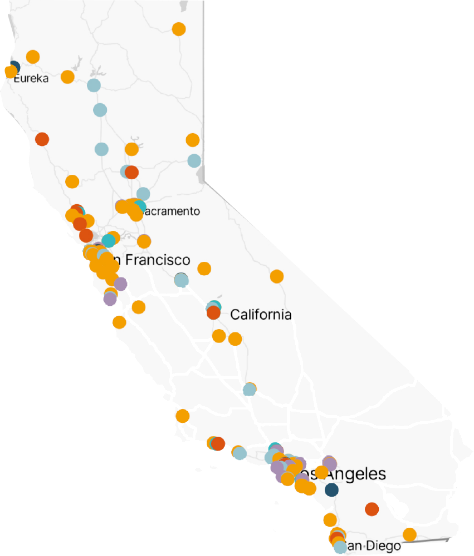
Between January 1, 2020 and March 31, 2023 (the most recent data available at the time this report was published), providers conducted more than 2.3 million ACE screenings of approximately 1.5 million unique Medi-Cal members. These screenings, which are reimbursed at $29 per screen, have generated more than $66 million in revenue to clinics serving predominantly low-income communities.
For more information about Medi-Cal screening rates, visit the ACEs Aware data reports web page and interactive maps that provide screening data by county.
Training
Becoming ACEs Aware in California is the flagship training program for the initiative and is based on the foundational principle that toxic stress is amenable to treatment. This free, two-hour, online course covers ACEs, toxic stress, ACE screening, toxic stress risk assessment, and trauma-informed care and provides health care teams evidence-based strategies to mitigate the toxic stress response.
After completing this training, qualified clinicians are certified to receive $29 for each eligible ACE screening they conduct. Since the launch of the ACEs Aware initiative, more than 35,360 individuals have completed the training, including approximately 17,100 Medi-Cal providers.
ACEs Aware has hosted more than 36 webinars and online courses that have been viewed more than 37,000 times. Topics include how to launch and sustain an ACE screening initiative in primary care clinics, ACE screening and trauma-informed care in reproductive health settings, and evidence-based strategies for mitigating toxic stress.
Community Investment
Since 2020, ACEs Aware has invested $65 million in clinics and communities across the state to support their local and regional approaches to preventing, identifying, and responding to ACEs and toxic stress. Through three distinct grant cycles, funding has been directed to Medi-Cal clinics, health care organizations, and community-based organizations throughout California to implement, strengthen, and sustain ACE screening and response initiatives and Trauma-Informed Networks of Care.
Supporting Clinical Innovations
ACEs Aware recognizes that there is no one-size-fits-all approach to clinical practices for implementing an ACE screening and response initiative. To that end, a key aspect of ACEs Aware’s work has been to support academic pilot projects examining innovative approaches to preventing, identifying, and responding to ACEs and toxic stress in different settings and with different patient populations.
Over the last two years, UCLA and UCSF have led 10 pilots at UCLA and 11 at UCSF, collaborating across academic and clinical departments and with partners in the community. The pilot projects are designed to fill gaps in knowledge and resources necessary to inform ACEs Aware trainings, clinical protocols and guidelines, and recommendations for evidence-based strategies to mitigate toxic stress.

As we continue efforts to advance screening initiatives, we also continue to improve our understanding of the impact of ACE screening and response activities on health care delivery and health outcomes and have evaluations underway to produce data to inform future phases of the initiative. Early findings in LA County suggest that ACE screening and response initiatives are advancing ACEs Aware and DHCS statewide goals to improve quality of care and reduce health disparities for the most vulnerable Californians, such as increasing access to health care services for patients screened for ACEs and identified as high risk for toxic stress.
The Path Ahead
The ACEs Aware initiative recognizes the disproportionate prevalence, impact, and burden of ACEs, cumulative adversity, and toxic stress on historically marginalized populations. The initiative is committed to supporting California’s health equity goals and through programs such as community grants, ensuring that ACE screening and response activities are fully integrated and aligned with Medi-Cal’s expanded benefits, workforce, and services offered through California Advancing and Innovating Medi-Cal (CalAIM) and other Medi-Cal transformation initiatives.
Bold Goals 50x2025
Although ACEs Aware has made considerable progress, more work lies ahead in the effort to prevent and mitigate the impact of ACEs and toxic stress on current and future generations of Californians.
As we look ahead in 2024 and beyond, ACEs Aware envisions both broader and deeper engagement with local and statewide efforts to drive equitable, seamless, person-centered, and whole family care for California’s diverse Medi-Cal populations.